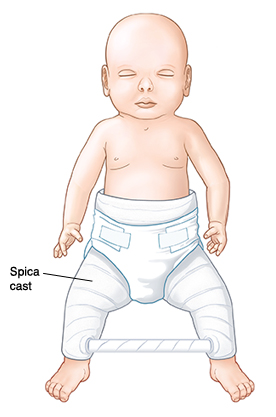
When Your Child Needs a Spica Cast
Your child needs a spica cast. This is a cast that covers the child’s lower body. It's used to treat problems, such as broken bones (fractures) in the hips or thighs. Or hip dislocation (developmental dysplasia of the hip or DDH). A spica cast reaches from the chest over the hips and down 1 or both legs. It has a cutout at the groin for toileting. A bar may connect the legs to make the cast more stable. A spica cast is applied by an orthopedist. This is a healthcare provider specializing in treating bone and joint problems. This is often done in an operating room. Your child will wear the cast for 4 to 12 weeks.
When is a spica cast needed?
 |
| You will be given instructions on how to care for your child while he or she is in a spica cast. |
A spica cast is used to stabilize and protect the hip or thigh area for a set time. This helps problems or injuries in these areas heal. A spica cast may be used after the following:
-
A thighbone (femur) fracture
-
Hip or pelvis problems or fractures
-
Dislocation (pushing out of place) of the hip joint
-
Certain surgeries, such as a tendon release
Caring for your child
You'll be given specific instructions for caring for your child and the spica cast. Here are some guidelines:
-
Inspect the cast and your child regularly for:
-
Sharp areas or rough spots near skin.
-
Skin that is red, irritated, or sore.
-
A skin rash around or under the cast.
-
Skin that is numb or changes color.
-
Keep the cast dry. Don’t let water get under the cast. Bathe and clean your child with sponge baths, as instructed. Clean the groin area carefully.
-
Tape around the edges of the groin opening of the cast. This helps the cast stay clean. Many parents use moleskin or duct tape.
-
Diaper your child as instructed by the healthcare provider. Often, a diaper is put on underneath the opening of the spica cast. Then another larger diaper is placed over the cast. A woman’s menstrual pad (sanitary napkin) can be used on the inside diaper to increase absorbency. Change diapers often to prevent skin breakdown and soiling of the cast. You'll likely have to help a toilet-trained child use the toilet. A bed pan or urinal (for boys) may be needed for older children.
-
Just after the cast is put on, limit your child’s activity to let the injury stabilize. Gentle activities are encouraged. These include board games, reading, listening to music, puzzles, crafts, and video games. Your child’s provider can give you specific activity guidelines for your child while the cast is in place.
-
Put your child’s clothing on over the cast. Loose or larger-sized clothing works best, such as large sweat pants or 1-piece bodysuits for infants. Larger clothing can be cut and velcro applied to make it easier to dress the child.
-
Change a child's position often, about every 2 to 4 hours. Consider using a bean bag chair, pillows, or a recliner for ease of positioning the child.
-
To get around, older children may need a reclining wheelchair, which you can get at a medical supply store. Younger children can be placed in an adjustable stroller or wagon. Remember to always use safety straps.
When to call the healthcare provider
Call your child's healthcare provider right away if your child has any of these:
-
Fever (see “Fever and children” below)
-
Chills
-
Skin around the cast is red, irritated, or sore
-
The toes change color or feel very cool to touch
-
Your child can't move or wiggle their toes
-
A skin rash develops near or under the cast
-
Your child complains that a spot under the cast hurts or burns
-
Your child’s toes are numb or tingly
-
Your child has pain that isn't eased by raising the legs and using acetaminophen or other prescribed pain medicine
-
The cast develops any breaks, cracks, or sharp spots
-
If something falls down into the cast and becomes stuck
-
The cast gets wet or very dirty, or the crotch opening gets soiled with stool or urine
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The healthcare provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older