Medulloblastoma (Child)
Medulloblastoma is a rare type of brain cancer. It can occur in children and young adults, but is more common in young children.
How a medulloblastoma grows
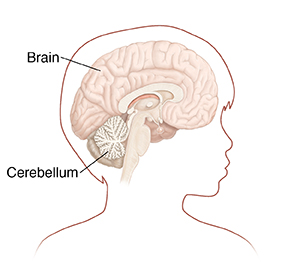
Medulloblastoma is a primary brain tumor. This means it starts in the brain instead of going to the brain from somewhere else in the body. This type of tumor grows fast. It starts in the cerebellum, near the back of the brain. The cerebellum controls balance and coordination.
This type of tumor may spread (metastasize) in the brain and spinal cord. Medulloblastoma very rarely spreads to other parts of the body, like the bone or lung. A tumor that has spread is harder to treat. And even a small tumor in the brain can press against other parts of the brain and cause problems.
Types of medulloblastoma
Medulloblastoma has been grouped into different types based on how the tumor cells look under the microscope. But most healthcare providers categorize them into four main subtypes based on the genetic features of the tumor cells. The subtypes of medulloblastoma are:
-
WNT-activated
-
SHH-activated (sonic hedgehog)
-
Group 3 (non-WNT/non-SHH)
-
Group 4 (non-WNT/non-SHH)
Some subgroups are harder to cure than others. Because of this, different subgroups may be treated differently. Your child's provider can tell you more about the type of medulloblastoma your child has and what this means.
What causes medulloblastoma?
Researchers are still learning why this kind of brain tumor grows. Certain genetic changes that are passed down through families may cause the tumor to grow. These include Gorlin (nevoid basal cell carcinoma) syndrome and Turcot syndrome. But these account for a small number of people with the tumor. Most people with medulloblastoma do not have a genetic disorder.
Symptoms of medulloblastoma
Symptoms tend to start slowly and get worse as the tumor grows. They depend on where the tumor is in the brain.
Headache is common. A brain tumor can block the normal flow of cerebral spinal fluid. This leads to increased intracranial pressure. This pressure in the skull may cause headache, nausea, vomiting, and dizziness. Because the tumor grows in the cerebellum, it may affect balance and coordination early on.
Symptoms of medulloblastoma may include:
-
Headache, especially in the morning
-
Nausea and vomiting, which may be worst in the morning
-
Seizures
-
Changes in ability to think or confusion
-
Balance problems or clumsiness
-
Dizziness
-
Double vision, blurred vision, or other eye problems
-
Tiredness (fatigue)
Diagnosing medulloblastoma
The healthcare provider will ask about your child’s health history and symptoms. The provider may also ask about your family’s health history. They will do a physical exam, including a neurologic exam. The provider may ask your child to do simple things like walk, touch finger to nose, hold their hands out, or follow a light with their eyes. If a provider suspects a brain tumor, your child may need tests, such as:
-
MRI of the brain and spinal cord with a contrast medium (gadolinium)
-
CT scan with contrast medium
-
Spinal tap (lumbar puncture) to look for tumor cells in CSF
Your child should see a provider that treats brain tumors. This may be a neurologist, neurosurgeon, or neuro-oncologist. A surgeon may need to remove the tumor so that it can be tested in a lab. The provider will explain your child’s test results, including the pathology report from the lab. This report tells the exact type, size, rate of growth, and other information about your child’s tumor.
Treatment for medulloblastoma
The healthcare team will work with you to decide the best treatment plan for your child. The plan depends on the type of tumor, tumor risk, and where it is. Your child's first treatment will likely be surgery. This is done to remove as much of the cancer as safely possible. The tumor is sent to a lab for testing to learn more about the cancer. After surgery, your child may need radiation therapy. Chemotherapy is also a likely part of treatment for medulloblastoma. Your child may get high-dose chemotherapy with stem cell transplantation if the tumor comes back after treatment.. It depends on the tumor's subtype and the amount of spread.
If your child has increased intracranial pressure, they may need a shunt. This is a thin, flexible tube put in the skull to help drain excess CSF. Your child will need to have follow-up MRI scans done to see how well treatment is working.
Ask your healthcare provider if a clinical trial is a possible choice for your child to participate in.
Possible complications of treatment
Your child's healthcare team will talk with you about possible complications of treatment, which may include:
-
Short-term brain damage from surgery and radiation, which may cause problems with thinking, learning, and paying attention
-
Cerebellar mutism syndrome (posterior fossa syndrome). This might occur after surgery and can last for months or years. Signs of it include:
-
Delayed talking
-
Trouble swallowing and eating
-
Loss of balance and trouble walking
-
Loss of muscle tone
-
Personality changes and mood swings
-
Nausea, vomiting, and tiredness (fatigue) from radiation, chemotherapy, or both
-
Infertility
-
Slowed growth and development
-
Hearing loss
-
Increased risk for other cancers later in life
-
Increased risk for stroke later in life
Follow-up care
Most children with medulloblastoma have good outcomes. But in some cases, the tumor comes back after treatment. To watch for this and long-term treatment complications, your child will need to see the cancer care team regularly. They will likely need to have follow-up MRI scans in the weeks after surgery and then a few times a year after that. Your child may also benefit from long-term therapy from healthcare providers who focus on childhood cancer survivors.